Medically reviewed by Mr Hyder Ridha (GMC: 6076878), Consultant Plastic, Reconstructive & Aesthetic Surgeon.


Breast Reconstruction
Breast reconstruction restores the shape, size, and appearance of one or both breasts following breast cancer treatment, to help women feel more comfortable with their bodies.
Breast reconstruction is a transformative surgical procedure that can help women regain their sense of wholeness and confidence following a mastectomy or lumpectomy.
We’ll explore the various types of breast reconstruction our London and Hertfordshire clinics offer, including the different surgical techniques available, the benefits and the recovery process.
We’ll also discuss the costs associated with breast reconstruction surgery in the UK.
Breast reconstruction restores the shape, size, and appearance of one or both breasts following breast cancer treatment, to help women feel more comfortable with their bodies.
Breast Reconstruction At a Glance
Surgery time
Implant reconstruction 2-3 hours; Autologous 6-8 hours
Anaesthesia
General anaesthetic
Hospital stay
Implant day case; Autologous 3-5 days
Recovery
Implant 2 weeks; Autologous 8 weeks
Bras and garments
Support garment for 6 weeks
Sleeping on back
4 weeks
Sexual activity
Implant 4 weeks; Autologous 4 weeks
Scar healing
2 weeks

What is Breast Reconstruction Surgery?
Breast reconstruction is a surgical procedure designed to restore the shape, size, and appearance of one or both breasts following breast cancer treatment.
The goal is to help women feel more confident and comfortable with their bodies, allowing them to move forward with their lives.
There are several different techniques, including implant-based reconstruction and autologous tissue-based reconstruction.
Types of reconstruction
- Implant-based breast reconstruction:
Implant-based reconstruction is the most common technique. It involves placing an implant in front of, or partly behind the chest muscle to create a new breast mound. In some cases, a tissue expander may be used initially to help stretch the skin and create space for an implant. - Autologous tissue-based breast reconstruction:
Also known as flap reconstruction, is where your own tissue is used to create a new breast mound. Common flap techniques include the DIEP flap (deep inferior epigastric artery perforator flap), which uses tissue from the tummy; the PAP flap (profunda artery perforator flap), which uses tissue from the inner thigh; and the latissiumus dorsi flap, which uses tissue from the back. These all provide a more natural-looking and feeling breast.

Understanding why other women choose to have breast reconstruction, the associated risks and often lifechanging benefits can help you to feel more confident about your decision. This guide helps you explore the topic.
Why Choose Breast Reconstruction Surgery?
For many women the restoration of their breast symbolises the end of their cancer treatment and the beginning of a new chapter with a restored sense of wholeness and confidence.
You might like to consider the following factors when deciding on the best breast reconstruction technique for you:
- Your overall health
- The size and shape of any remaining breast tissue as well as the unaffected breast
- Your personal preferences
Some women opt for implant-based reconstruction, which involves the placement of an implant to create a new breast mound. Others opt for autologous tissue-based reconstruction, which uses your own tissue, taken usually from the tummy, back, thigh or buttock, to recreate the breast.
Benefits of Breast Reconstruction
Breast reconstruction is a powerful and life-changing procedure that can help women regain their confidence and sense of wholeness after breast cancer treatment.
Open communication with your surgeon is essential, and feeling confident in your choice will support the best possible outcome.
- Improved self-confidence
Increased self-esteem and self-confidence as a result of regaining breast appearance. - Customised outcomes
You can choose the size and shape of the reconstruction to achieve your unique desired look. - Long-lasting results
The outcomes of breast reconstruction are typically long-lasting, providing enduring benefits.
Risks of Breast Reconstruction Surgery
Breast reconstruction carries certain risks, and it is important to understand these potential complications:
- Scarring
Surgical incisions can result in visible scars, although every effort is made to minimise their appearance. - Infection
All surgery carries a risk of infection, although these are relatively rare. - Implant-related issues
Breast implants may rupture, leak or develop capsular contracture, which may require further surgical intervention. - Changes in sensation
Some patients may experience temporary or permanent changes in breast sensation, including numbness or hypersensitivity. - Anaesthesia risks
There are inherent risks associated with anaesthesia, which the surgical and anaesthetic team will discuss during your preoperative evaluation.

Who is a good candidate?
Choosing to have breast reconstruction surgery is a highly personal decision. In essence any breast cancer survivor who is in good health is a good candidate.


Psychologically prepared
You are emotionally ready to embark on a reconstruction and have appropriate support at home for your journey
Be in good health
You do not have additional medical conditions or other illnesses that may increase the risks of an anaesthetic and/or impair healing
Realistic expectations
You have a positive outlook and realistic goals for restoring your breast and body image

Book a Consultation
Take the first step toward your ideal look by booking a consultation with our expert surgeon.


Understanding what breast reconstruction surgery involves, can help you feel more confident and prepared for your journey. The procedure is carefully planned to achieve the results you desire, whilst keeping your safety and comfort paramount. From your initial consultation to recovery, each step is designed to offer a smooth experience. We outline below what you can expect from the process.
Consultation
Our highly skilled surgeon, Mr Hyder Ridha, possesses extensive expertise and experience in performing breast reconstruction procedures, ensuring your safety and delivering exceptional results. He will conduct the consultation personally where your goals are determined, the types of reconstruction explained, and all potential risks are discussed. He will also ensure you are prepared for surgery to ensure your best possible outcome through advice such as stopping smoking and avoiding certain medications.
How Breast Reconstruction Surgery Is Performed
- Anaesthesia
The procedure is performed under general anaesthetic. - Determining the reconstruction method
The surgical approach varies depending on whether you choose an implant-based reconstruction or an autologous tissue-based (flap) reconstruction. - Implant-based reconstruction
A saline or silicone implant is placed either in front of, or partly behind, the chest muscle to create a new breast mound. - Autologous (flap) reconstruction
Your own tissue is used to create a new breast mound.
This is a more complex procedure that involves microsurgical techniques.
Breast Reconstruction Recovery Timeline
| Varies by technique | Recovery time depends on whether you undergo implant-based or autologous breast reconstruction. |
| Implant-based reconstruction | This can be performed as a daycase. Total expected recovery time is approximately 2 weeks. |
| Autologous reconstruction | A more complex procedure that requires a 3–5 night hospital stay, with recovery taking up to 6 weeks. |
| Postoperative care | Following postoperative advice and attending all follow-up appointments is essential for achieving the best possible outcome. |

Breast Reconstruction Procedure Video
Take a look at the video to understand what you can expect from a breast reconstruction procedure.

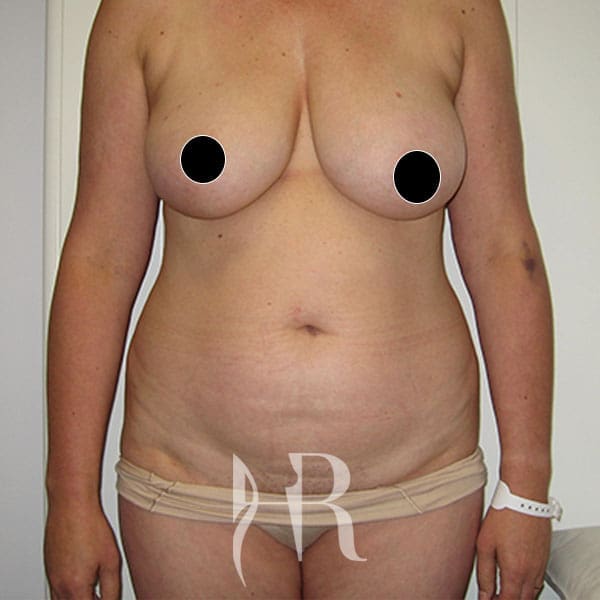
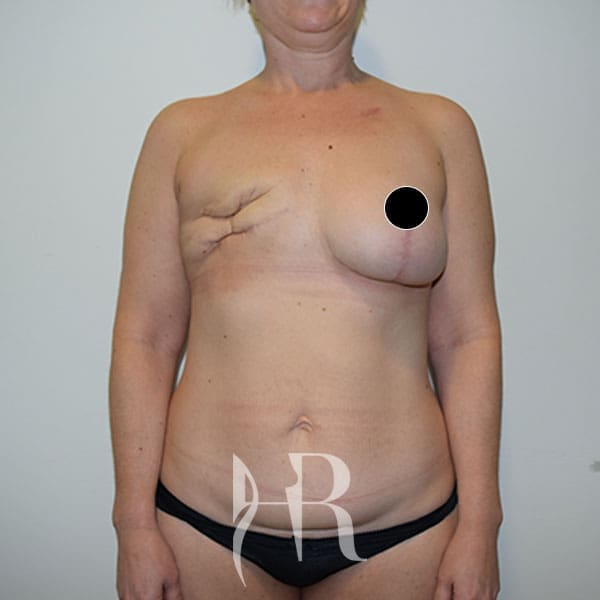
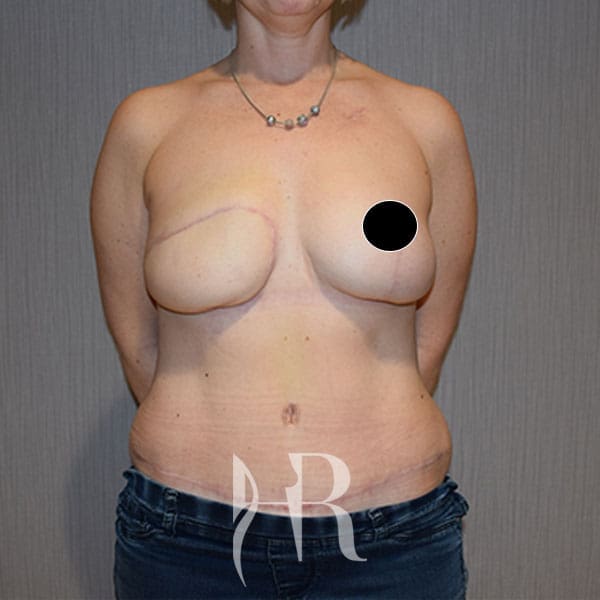
Breast Reconstruction Results
The choice to have breast reconstruction surgery is a very personal decision. It can be useful to see previous Breast Reconstruction before and after image results to understand what you can expect and help you to make up your mind.
What is the cost of breast reconstruction surgery?
Prices from
£25,000
The cost of breast reconstruction surgery varies depending on the surgeon’s experience, the specific type of reconstruction technique used, and the complexity of the reconstruction procedure. To ensure you receive the best possible care and results, it’s essential to understand the cost of the surgery and budget accordingly. Keep in mind that some or all the costs may be covered by your insurance provider, depending on your policy and the medical necessity of the procedure. Be sure to discuss your financial options with our team*. You can find more information on our pricing and payment plans pages*, or please get in touch with our team and we’ll gladly discuss your options.

FAQs
Is it worth having breast reconstruction?
The decision to have breast reconstruction after a mastectomy is a very personal one and should be made with careful consideration.
It can help restore shape, symmetry and size to the breast after a mastectomy, which can provide a boost to self-confidence and help patients feel more like themselves. Ultimately, though, it is up to you to decide if breast reconstruction is right for you.
What is the success rate of breast surgery to reconstruct the breast?
The success rate is very high, with more than 95% of patients reporting satisfaction with the results. The success rate depends on the type of reconstruction chosen, your anatomy, and the skill of the surgeon.
How long do you have to wait for breast reconstruction?
Breast reconstruction can be offered at the time of the surgical treatment of the breast cancer, known as an immediate reconstruction, or can be performed as a separate procedure at a later date, known as a delayed reconstruction.
The decision as to whether to undergo an immediate or delayed reconstruction is determined by patient preference and factors related to the cancer treatment
Can you have breast implants after you have had breast cancer?
Yes, you can have breast implants (breast augmentation) after you have had breast cancer and completed chemotherapy and radiation therapy. However, the decision to have breast implants should be discussed with your doctor first.
Depending on your circumstances, your doctor may advise against having breast implants.
Is reconstructive surgery the same as microvascular surgery?
- Reconstructive surgery
Reconstructive surgery is the process of restoring form and function to parts of the body that have been damaged due to injury, trauma, or disease. - Microvascular surgery
Microvascular surgery is a specialised technique used within reconstructive surgery.
It involves connecting very small blood vessels (less than 2 mm in diameter) to help reconstruct parts of the body.
When should breast reconstruction surgery be performed?
- Depends on individual circumstances
The timing of breast reconstruction surgery depends on your specific circumstances, overall health, and personal preferences. - Immediate reconstruction
Some women choose to have reconstruction performed immediately after their mastectomy or lumpectomy. - Delayed reconstruction
Others opt for delayed reconstruction, which takes place several months or even years after breast cancer surgery.
Will I have any sensation in my reconstructed breast?
Breast sensation after reconstruction varies depending on the specific technique used and the extent of the surgery. Some women may experience a decrease in sensation, while others may regain some or all their breast sensation over time. It’s essential to discuss this with your surgeon and set realistic expectations for your post-surgery experience.
Can I still have mammograms after breast reconstruction?
Yes, mammograms can still be performed on a reconstructed breast, though the frequency and type of imaging may vary depending on the specific reconstruction technique used. Discuss this with your surgeon and follow their recommendations.
Can breast reconstruction affect cancer recurrence or detection?
Breast reconstruction does not impact your ability to detect a recurrence of breast cancer or have any impact on cancer recurrence rates. However, it’s essential to continue regular breast cancer screening and follow-up care as recommended by your healthcare team.
Access essential resources & information at your convenience.
Browse our collection of brochures, guides, and forms to learn more about our procedures, prepare for your visit, or explore your options. Simply download what you need to get started.

Breast Implant Associated Anaplastic

Breast Implant Illness (BII)